What Are The Causes Of Heel Pain
Overview

Heel pain is one of the most common conditions to affect the foot. It is usually felt as an intense pain when the affected heel is used. The pain is usually worse when you get out of bed in the morning or after a long period of activity. In most cases, only one heel is affected. After walking, the pain usually improves. However, it is common for it to be painful when you first take a step after a period of rest. The pain often worsens by the end of the day. Most cases of heel pain are caused by damage and thickening of the plantar fascia. Sometimes, the surrounding tissue and the heel bone also become inflamed (swollen).
Causes
The plantar fascia spans the long arch of the foot from the heel to the base of the toes, where it blends with the soft tissues, then anchoring to the base of the toes. Plantar Fascia. The plantar fascia is a common cause of heel pain. As the bony attachment at the heel is considered the plantar fascia?s ?weak spot?, the patient will present with pain at the heel, mainly on the inside. The most common predisposing factor to this condition is the pronating (flattening feet) - 52% - whilst there is also some evidence that a very high arch, in a rigid foot (pes cavus), also was reasonably common - 42%.
Symptoms
Usually when a patient comes in they?ll explain that they have severe pain in the heel. It?s usually worse during the first step in the morning when they get out of bed. Many people say if they walk for a period of time, it gets a little bit better. But if they sit down and get back up, the pain will come back and it?s one of those intermittent come and go types of pain. Heel pain patients will say it feels like a toothache in the heel area or even into the arch area. A lot of times it will get better with rest and then it will just come right back. So it?s one of those nuisance type things that just never goes away. The following are common signs of heel pain and plantar fasciitis. Pain that is worse first thing in the morning. Pain that develops after heavy activity or exercise. Pain that occurs when standing up after sitting for a long period of time. Severe, toothache type of pain in the bottom of the heel.
Diagnosis
After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including. Whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair. Your doctor will examine you, including. An evaluation of your gait. While you are barefoot, your doctor will ask you to stand still and to walk in order to evaluate how your foot moves as you walk. An examination of your feet. Your doctor may compare your feet for any differences between them. Then your doctor may examine your painful foot for signs of tenderness, swelling, discoloration, muscle weakness and decreased range of motion. A neurological examination. The nerves and muscles may be evaluated by checking strength, sensation and reflexes. In addition to examining you, your health care professional may want to examine your shoes. Signs of excessive wear in certain parts of a shoe can provide valuable clues to problems in the way you walk and poor bone alignment. Depending on the results of your physical examination, you may need foot X-rays or other diagnostic tests.
Non Surgical Treatment
Essentially rest from aggravating activity, physiotherapy treatment to alleviate the inflammatory component, stretching the tight calf, strengthening up of the intrinsic muscles of the foot e.g. tissue scrunch, picking up pens etc. and correction of biomechanical problems in the foot e.g. orthotics. Sometimes, a heel cup or pad to relieve pressure - a donut type pad may be helpful. Strapping has been shown to be helpful, especially in circumstances where the patient can?t wear orthotics - the foot is strapped to help support the arch. There has been limited success with cortisone injections or surgery and the latter is very rarely required.
Surgical Treatment
Surgery to correct heel pain is generally only recommended if orthotic treatment has failed. There are some exceptions to this course of treatment and it is up to you and your doctor to determine the most appropriate course of treatment. Following surgical treatment to correct heel pain the patient will generally have to continue the use of orthotics. The surgery does not correct the cause of the heel pain. The surgery will eliminate the pain but the process that caused the pain will continue without the use of orthotics. If orthotics have been prescribed prior to surgery they generally do not have to be remade.
deelsonheels
Prevention

Make sure you wear appropriate supportive shoes. Don't over-train in sports. Make sure you warm up, cool down and undertake an exercise regime that helps maintain flexibility. Manage your weight, obesity is a factor in causing plantar fasciitis. Avoid walking and running on hard surfaces if you are prone to pain. You should follow the recognized management protocol "RICED" rest, ice, compression, elevation and diagnosis. Rest, keep off the injured ankle as much as possible. Ice, applied for 20 minutes at a time every hour as long as swelling persists. Compression, support the ankle and foot with a firmly (not tightly) wrapped elastic bandage. Elevation, keep foot above heart level to minimize bruising and swelling. Diagnosis. Consult a medical professional (such as a Podiatrist or doctor) especially if you are worried about the injury, or if the pain or swelling gets worse. If the pain or swelling has not gone down significantly within 48 hours, also seek treatment. An accurate diagnosis is essential for proper rehabilitation of moderate to severe injuries.

Heel pain is one of the most common conditions to affect the foot. It is usually felt as an intense pain when the affected heel is used. The pain is usually worse when you get out of bed in the morning or after a long period of activity. In most cases, only one heel is affected. After walking, the pain usually improves. However, it is common for it to be painful when you first take a step after a period of rest. The pain often worsens by the end of the day. Most cases of heel pain are caused by damage and thickening of the plantar fascia. Sometimes, the surrounding tissue and the heel bone also become inflamed (swollen).
Causes
The plantar fascia spans the long arch of the foot from the heel to the base of the toes, where it blends with the soft tissues, then anchoring to the base of the toes. Plantar Fascia. The plantar fascia is a common cause of heel pain. As the bony attachment at the heel is considered the plantar fascia?s ?weak spot?, the patient will present with pain at the heel, mainly on the inside. The most common predisposing factor to this condition is the pronating (flattening feet) - 52% - whilst there is also some evidence that a very high arch, in a rigid foot (pes cavus), also was reasonably common - 42%.
Symptoms
Usually when a patient comes in they?ll explain that they have severe pain in the heel. It?s usually worse during the first step in the morning when they get out of bed. Many people say if they walk for a period of time, it gets a little bit better. But if they sit down and get back up, the pain will come back and it?s one of those intermittent come and go types of pain. Heel pain patients will say it feels like a toothache in the heel area or even into the arch area. A lot of times it will get better with rest and then it will just come right back. So it?s one of those nuisance type things that just never goes away. The following are common signs of heel pain and plantar fasciitis. Pain that is worse first thing in the morning. Pain that develops after heavy activity or exercise. Pain that occurs when standing up after sitting for a long period of time. Severe, toothache type of pain in the bottom of the heel.
Diagnosis
After you have described your foot symptoms, your doctor will want to know more details about your pain, your medical history and lifestyle, including. Whether your pain is worse at specific times of the day or after specific activities. Any recent injury to the area. Your medical and orthopedic history, especially any history of diabetes, arthritis or injury to your foot or leg. Your age and occupation. Your recreational activities, including sports and exercise programs. The type of shoes you usually wear, how well they fit, and how frequently you buy a new pair. Your doctor will examine you, including. An evaluation of your gait. While you are barefoot, your doctor will ask you to stand still and to walk in order to evaluate how your foot moves as you walk. An examination of your feet. Your doctor may compare your feet for any differences between them. Then your doctor may examine your painful foot for signs of tenderness, swelling, discoloration, muscle weakness and decreased range of motion. A neurological examination. The nerves and muscles may be evaluated by checking strength, sensation and reflexes. In addition to examining you, your health care professional may want to examine your shoes. Signs of excessive wear in certain parts of a shoe can provide valuable clues to problems in the way you walk and poor bone alignment. Depending on the results of your physical examination, you may need foot X-rays or other diagnostic tests.
Non Surgical Treatment
Essentially rest from aggravating activity, physiotherapy treatment to alleviate the inflammatory component, stretching the tight calf, strengthening up of the intrinsic muscles of the foot e.g. tissue scrunch, picking up pens etc. and correction of biomechanical problems in the foot e.g. orthotics. Sometimes, a heel cup or pad to relieve pressure - a donut type pad may be helpful. Strapping has been shown to be helpful, especially in circumstances where the patient can?t wear orthotics - the foot is strapped to help support the arch. There has been limited success with cortisone injections or surgery and the latter is very rarely required.
Surgical Treatment
Surgery to correct heel pain is generally only recommended if orthotic treatment has failed. There are some exceptions to this course of treatment and it is up to you and your doctor to determine the most appropriate course of treatment. Following surgical treatment to correct heel pain the patient will generally have to continue the use of orthotics. The surgery does not correct the cause of the heel pain. The surgery will eliminate the pain but the process that caused the pain will continue without the use of orthotics. If orthotics have been prescribed prior to surgery they generally do not have to be remade.
deelsonheels
Prevention

Make sure you wear appropriate supportive shoes. Don't over-train in sports. Make sure you warm up, cool down and undertake an exercise regime that helps maintain flexibility. Manage your weight, obesity is a factor in causing plantar fasciitis. Avoid walking and running on hard surfaces if you are prone to pain. You should follow the recognized management protocol "RICED" rest, ice, compression, elevation and diagnosis. Rest, keep off the injured ankle as much as possible. Ice, applied for 20 minutes at a time every hour as long as swelling persists. Compression, support the ankle and foot with a firmly (not tightly) wrapped elastic bandage. Elevation, keep foot above heart level to minimize bruising and swelling. Diagnosis. Consult a medical professional (such as a Podiatrist or doctor) especially if you are worried about the injury, or if the pain or swelling gets worse. If the pain or swelling has not gone down significantly within 48 hours, also seek treatment. An accurate diagnosis is essential for proper rehabilitation of moderate to severe injuries.
What Can You Do About Fallen Arches?
Overview
It is rare to find someone who walks with both feet in perfect alignment. Often we walk on the inside or outsides of our feet, or with our toes or heels rotated inward. These typical walking patterns can cause many problems not just with the feet but also for the whole body as the alignment of the feet sets the foundation for the whole body?s alignment. One of the most common effects of improper alignment is known as flatfoot, or fallen arches.
Causes
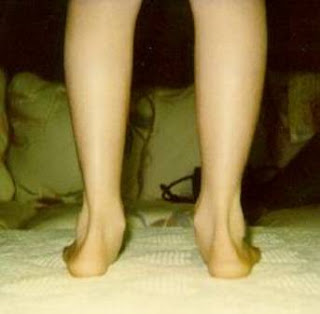
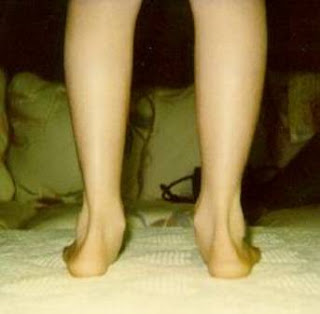
As discussed above, many health conditions can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to hold up the arch and support your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use.
Symptoms
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
pes planus exercises
Non Surgical Treatment
Most cases of flatfeet do not require treatment. However, if there is pain, or if the condition is caused by something other than normal development, there are several treatment options. Self-care options include rest, choosing non-weight-bearing exercise (e.g., swimming, cycling), weight loss, and avoiding high heels. Flexible flatfeet with some pain can be relieved with the use of orthotics-shoe inserts that support the arch-and/or heel wedges (in some cases). If pronation is a factor, special shoes can be worn that lift the arch and correct the inward leaning. Physical therapy may also be prescribed to stretch or lengthen the heel cord and other tendons. For rigid or inflexible flatfeet, treatment varies depending on the cause. Tarsal coalition if often treated with rest and the wearing of a cast. If this is ineffective, surgery can be done to separate the bones or to reset the bones into a correct position. If the flatfoot is caused by an injury to the tendons in the foot or ankle, rest, anti-inflammatory medications (e.g., ibuprofen), and the use of shoe inserts and ankle braces often relieve symptoms. In severe cases, surgery is performed to repair the tendon or to fuse some joints in the foot into a corrected position to reduce stress on the tendon. The prognosis after surgery is generally good. Complications include pain and some loss of ankle motion, especially when trying to turn the foot in or out. This may be improved with physical therapy.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Flat feet or Fallen Arches cannot be prevented due to congenital of nature or from underlying disease process; however, painful symptoms and future pathology from Flat Feet or Fallen Arches may be prevented by the following. Continue to wear your orthotics for work and exercise to provide stability and maintain function of your feet. Footwear. Continue to wear supportive shoes to maximise the function of your orthotic and prevent excessive movement of the joints in your feet.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
It is rare to find someone who walks with both feet in perfect alignment. Often we walk on the inside or outsides of our feet, or with our toes or heels rotated inward. These typical walking patterns can cause many problems not just with the feet but also for the whole body as the alignment of the feet sets the foundation for the whole body?s alignment. One of the most common effects of improper alignment is known as flatfoot, or fallen arches.
Causes
As discussed above, many health conditions can create a painful flatfoot. Damage to the posterior tibial tendon is the most common cause of AAFD. The posterior tibial tendon is one of the most important tendons of the leg. It starts at a muscle in the calf, travels down the inside of the lower leg and attaches to the bones on the inside of the foot. The main function of this tendon is to hold up the arch and support your foot when you walk. If the tendon becomes inflamed or torn, the arch will slowly collapse. Women and people over 40 are more likely to develop problems with the posterior tibial tendon. Other risk factors include obesity, diabetes, and hypertension. Having flat feet since childhood increases the risk of developing a tear in the posterior tibial tendon. In addition, people who are involved in high impact sports, such as basketball, tennis, or soccer, may have tears of the tendon from repetitive use.
Symptoms
People will have a very heavily dropped arch and it won?t affect them at all and people will have it slightly dropped and it could cause fierce problems. It could cause things like plantar fasciitis, it could cause heel spurs, desperate ball-of-the-foot pressure, or pressure on the big toe known as the hallux which causes discomfort in the foot. It will create problems upwards to the knees, hips and the back once you?re out of line.
Diagnosis
Podiatrists are trained in expertly assessing flat feet and identifying different risk factors and the causes for it. Initial assessment will begin with a detailed history attempting to find out if any underlying illness has resulted in this. A detailed clinical examination normally follows. The patient may be asked to perform certain movements such as walking or standing on their toes to assess the function of the foot. Footwear will also be analysed to see if there has been excessive wear or if they are contributing to the pronation of the foot. To assess the structure of the foot further, the podiatrist may perform certain x-rays to get a detailed idea of the way the bones are arranged and how the muscle tissues may be affecting them. It also helps assess any potential birth defects in a bit more detail.
pes planus exercises
Non Surgical Treatment
Most cases of flatfeet do not require treatment. However, if there is pain, or if the condition is caused by something other than normal development, there are several treatment options. Self-care options include rest, choosing non-weight-bearing exercise (e.g., swimming, cycling), weight loss, and avoiding high heels. Flexible flatfeet with some pain can be relieved with the use of orthotics-shoe inserts that support the arch-and/or heel wedges (in some cases). If pronation is a factor, special shoes can be worn that lift the arch and correct the inward leaning. Physical therapy may also be prescribed to stretch or lengthen the heel cord and other tendons. For rigid or inflexible flatfeet, treatment varies depending on the cause. Tarsal coalition if often treated with rest and the wearing of a cast. If this is ineffective, surgery can be done to separate the bones or to reset the bones into a correct position. If the flatfoot is caused by an injury to the tendons in the foot or ankle, rest, anti-inflammatory medications (e.g., ibuprofen), and the use of shoe inserts and ankle braces often relieve symptoms. In severe cases, surgery is performed to repair the tendon or to fuse some joints in the foot into a corrected position to reduce stress on the tendon. The prognosis after surgery is generally good. Complications include pain and some loss of ankle motion, especially when trying to turn the foot in or out. This may be improved with physical therapy.
Surgical Treatment

Fallen arches may occur with deformities of the foot bones. Tarsal coalition is a congenital condition in which the bones of the foot do not separate from one another during development in the womb. A child with tarsal coalition exhibits a rigid flat foot, which can be painful, notes the patient information website eOrthopod. Surgery may prove necessary to separate the bones. Other foot and ankle conditions that cause fallen arches may also require surgery if noninvasive treatments fail to alleviate pain and restore normal function.
Prevention
Flat feet or Fallen Arches cannot be prevented due to congenital of nature or from underlying disease process; however, painful symptoms and future pathology from Flat Feet or Fallen Arches may be prevented by the following. Continue to wear your orthotics for work and exercise to provide stability and maintain function of your feet. Footwear. Continue to wear supportive shoes to maximise the function of your orthotic and prevent excessive movement of the joints in your feet.
After Care
Patients may go home the day of surgery or they may require an overnight hospital stay. The leg will be placed in a splint or cast and should be kept elevated for the first two weeks. At that point, sutures are removed. A new cast or a removable boot is then placed. It is important that patients do not put any weight on the corrected foot for six to eight weeks following the operation. Patients may begin bearing weight at eight weeks and usually progress to full weightbearing by 10 to 12 weeks. For some patients, weightbearing requires additional time. After 12 weeks, patients commonly can transition to wearing a shoe. Inserts and ankle braces are often used. Physical therapy may be recommended. There are complications that relate to surgery in general. These include the risks associated with anesthesia, infection, damage to nerves and blood vessels, and bleeding or blood clots. Complications following flatfoot surgery may include wound breakdown or nonunion (incomplete healing of the bones). These complications often can be prevented with proper wound care and rehabilitation. Occasionally, patients may notice some discomfort due to prominent hardware. Removal of hardware can be done at a later time if this is an issue. The overall complication rates for flatfoot surgery are low.
True Leg Length Discrepancy Test
Overview
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.
Causes
Limb-length conditions can result from congenital disorders of the bones, muscles or joints, disuse or overuse of the bones, muscles or joints caused by illness or disease, diseases, such as bone cancer, Issues of the spine, shoulder or hip, traumatic injuries, such as severe fractures that damage growth plates.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference.
Non Surgical Treatment
Whether or not treatment should be pursued depends on the amount of discrepancy. In general, no treatment (other than a heel life, if desired) should be considered for discrepancies under two centimeters. If the discrepancy measures between two and five centimeters, one might consider a procedure to equalize leg length. Usually, this would involve closure of the growth plate on the long side, thereby allowing the short side to catch up; shortening the long leg; or possibly lengthening the short leg.

how to increase height after 25
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
The bone is lengthened by surgically applying an external fixation device to the leg. The external fixator, a scaffold-like frame, is connected to the bone with wires, pins, or both. A small crack is made in the bone and the frame creates tension when the patient or family member turns its dial. This is done several times each day. The lengthening process begins approximately five to 10 days after surgery. The bone may lengthen 1 millimeter per day, or approximately 1 inch per month. Lengthening may be slower in a bone that was previously injured. It may also be slower if the leg was operated on before. Bones in patients with potential blood vessel abnormalities, such as cigarette smokers, may also need to be lengthened more slowly. The external fixator is worn until the bone is strong enough to support the patient safely. This usually takes about three months for each inch. Factors such as age, health, smoking and participation in rehabilitation can affect the amount of time needed.

Causes
Limb-length conditions can result from congenital disorders of the bones, muscles or joints, disuse or overuse of the bones, muscles or joints caused by illness or disease, diseases, such as bone cancer, Issues of the spine, shoulder or hip, traumatic injuries, such as severe fractures that damage growth plates.
Symptoms
The patient/athlete may present with an altered gait (such as limping) and/or scoliosis and/or low back pain. Lower extremity disorders are possibly associated with LLD, some of these are increased hip pain and degeneration (especially involving the long leg). Increased risk of: knee injury, ITB syndrome, pronation and plantar fascitis, asymmetrical strength in lower extremity. Increased disc or vertebral degeneration. Symptoms vary between patients, some patients may complain of just headaches.
Diagnosis
There are several orthopedic tests that are used, but they are rudimentary and have some degree of error. Even using a tape measure with specific anatomic landmarks has its errors. Most leg length differences can be seen with a well trained eye, but I always recommend what is called a scanagram, or a x-ray bone length study (see picture above). This test will give a precise measurement in millimeters of the length difference.
Non Surgical Treatment
Whether or not treatment should be pursued depends on the amount of discrepancy. In general, no treatment (other than a heel life, if desired) should be considered for discrepancies under two centimeters. If the discrepancy measures between two and five centimeters, one might consider a procedure to equalize leg length. Usually, this would involve closure of the growth plate on the long side, thereby allowing the short side to catch up; shortening the long leg; or possibly lengthening the short leg.

how to increase height after 25
Surgical Treatment
Large leg length inequalities can be treated by staged lengthenings or by simultaneous ipsilateral femoral and tibial lengthenings. Additionally, lengthenings can be combined with appropriately timed epiphysiodesis in an effort to produce leg length equality. Staged lengthenings are often used for congenital deficiencies such as fibular hemimelia, in which 15 cm or more may be needed to produce leg length equality. We typically plan for the final lengthening to be completed by age 13 or 14 years, and allow at least 3 years between lengthenings. Lengthening of both the tibia and femur simultaneously requires aggressive therapy and treatment of soft tissue contractures. Curran et al[57] reported the need for surgical release of soft tissue contractures in 3 of 8 patients treated with simultaneous ipsilateral femoral and tibial lengthenings. Lengthening over an IM nail can be done in an effort to decrease the amount of time the fixator needs to be worn and to prevent angular malalignment. This technique requires that the patient be skeletally mature and it carries a higher risk of osteomyelitis (up to 15%). Additionally, if premature consolidation occurs, a repeat corticotomy is more difficult.
What Is Mortons Neuroma
Overview
 Morton's neuroma is an enlarged nerve that usually occurs in the third interspace, which is between the third and fourth toes. To understand Morton's neuroma further, it may be helpful to look at the anatomy of the foot. Problems often develop in the third interspace because part of the lateral plantar nerve combines with part of the medial plantar nerve here. When the two nerves combine, they are typically larger in diameter than those going to the other toes. Also, the nerve lies in subcutaneous tissue, just above the fat pad of the foot, close to an artery and vein. Above the nerve is a structure called the deep transverse metatarsal ligament. This ligament is very strong, holds the metatarsal bones together, and creates the ceiling of the nerve compartment. With each step, the ground pushes up on the enlarged nerve and the deep transverse metatarsal ligament pushes down. This causes compression in a confined space.
Morton's neuroma is an enlarged nerve that usually occurs in the third interspace, which is between the third and fourth toes. To understand Morton's neuroma further, it may be helpful to look at the anatomy of the foot. Problems often develop in the third interspace because part of the lateral plantar nerve combines with part of the medial plantar nerve here. When the two nerves combine, they are typically larger in diameter than those going to the other toes. Also, the nerve lies in subcutaneous tissue, just above the fat pad of the foot, close to an artery and vein. Above the nerve is a structure called the deep transverse metatarsal ligament. This ligament is very strong, holds the metatarsal bones together, and creates the ceiling of the nerve compartment. With each step, the ground pushes up on the enlarged nerve and the deep transverse metatarsal ligament pushes down. This causes compression in a confined space.
Causes
Experts are not sure what exactly causes Morton's neuroma. It seems to develop as a result of irritation, pressure or injury to one of the digital nerves that lead to the toes, which triggers a body response, resulting in thickened nerve tissue (neuroma). Feet conditions/situations that can cause the bones to rub against a nerve include high-heeled shoes, especially those over 2 inches (5cm), or a pointed or tight toe box which squash the toes together. This is probably why the condition is much more common in females than in males. High-arched foot, people whose feet have high arches are much more likely to suffer from Morton's neuroma than others. Flat feet, the arch of the foot collapses. The entire sole of the foot comes into complete or near-complete contact with the ground. A bunion, a localized painful swelling at the base of the big toe, which enlarges the joint. Hammer toe, a deformity of the proximal interphalangeal joint of the second, third, or fourth toe causing it to be permanently bent. Some high-impact sporting activities including running, karate, and court sports. Any sport that places undue pressure on the feet. Injuries, an injury or other type of trauma to the foot may lead to a neuroma.
Symptoms
The most common symptom of Morton's neuroma is localized pain in the interspace between the third and fourth toes. It can be sharp or dull, and is worsened by wearing shoes and by walking. Pain usually is less severe when the foot is not bearing weight.
Diagnosis
If you suspect Morton?s Neuroma, it is essential that you confirm your suspicions by consulting with a podiatric physician. Don?t wait for the symptoms to go away for good (even if they tend to come and go). Also, remember that many conditions have similar symptoms, and only a professional can tell the difference.
Non Surgical Treatment
Wear shoes with plenty of room for the toes to move, low heels, and laces or buckles that allow for width adjustment. Wear shoes with thick, shock-absorbent soles, as well as proper insoles that are designed to keep excessive pressure off of the foot. High-heeled shoes over two inches tall should be avoided whenever possible because they place undue strain on the forefoot. Resting the foot and massaging the affected area can temporarily alleviate neuroma pain. Use an ice pack to help to dull the pain and improve comfort. Use over-the-counter shoe pads. These pads can relieve pressure around the affected area.
Surgical Treatment
If conservative treatments haven't helped, your doctor might suggest injections. Some people are helped by the injection of steroids into the painful area. In some cases, surgeons can relieve the pressure on the nerve by cutting nearby structures, such as the ligament that binds together some of the bones in the front of the foot. Surgical removal of the growth may be necessary if other treatments fail to provide pain relief. Although surgery is usually successful, the procedure can result in permanent numbness in the affected toes.
Prevention
Although the exact causes of neuromas are not completely known, the following preventive steps may help. Make sure your exercise shoes have enough room in the front part of the shoe and that your toes are not excessively compressed. Wear shoes with adequate padding in the ball of the foot. Avoid prolonged time in shoes with a narrow toe box or excessive heel height (greater than two inches).
 Morton's neuroma is an enlarged nerve that usually occurs in the third interspace, which is between the third and fourth toes. To understand Morton's neuroma further, it may be helpful to look at the anatomy of the foot. Problems often develop in the third interspace because part of the lateral plantar nerve combines with part of the medial plantar nerve here. When the two nerves combine, they are typically larger in diameter than those going to the other toes. Also, the nerve lies in subcutaneous tissue, just above the fat pad of the foot, close to an artery and vein. Above the nerve is a structure called the deep transverse metatarsal ligament. This ligament is very strong, holds the metatarsal bones together, and creates the ceiling of the nerve compartment. With each step, the ground pushes up on the enlarged nerve and the deep transverse metatarsal ligament pushes down. This causes compression in a confined space.
Morton's neuroma is an enlarged nerve that usually occurs in the third interspace, which is between the third and fourth toes. To understand Morton's neuroma further, it may be helpful to look at the anatomy of the foot. Problems often develop in the third interspace because part of the lateral plantar nerve combines with part of the medial plantar nerve here. When the two nerves combine, they are typically larger in diameter than those going to the other toes. Also, the nerve lies in subcutaneous tissue, just above the fat pad of the foot, close to an artery and vein. Above the nerve is a structure called the deep transverse metatarsal ligament. This ligament is very strong, holds the metatarsal bones together, and creates the ceiling of the nerve compartment. With each step, the ground pushes up on the enlarged nerve and the deep transverse metatarsal ligament pushes down. This causes compression in a confined space.Causes
Experts are not sure what exactly causes Morton's neuroma. It seems to develop as a result of irritation, pressure or injury to one of the digital nerves that lead to the toes, which triggers a body response, resulting in thickened nerve tissue (neuroma). Feet conditions/situations that can cause the bones to rub against a nerve include high-heeled shoes, especially those over 2 inches (5cm), or a pointed or tight toe box which squash the toes together. This is probably why the condition is much more common in females than in males. High-arched foot, people whose feet have high arches are much more likely to suffer from Morton's neuroma than others. Flat feet, the arch of the foot collapses. The entire sole of the foot comes into complete or near-complete contact with the ground. A bunion, a localized painful swelling at the base of the big toe, which enlarges the joint. Hammer toe, a deformity of the proximal interphalangeal joint of the second, third, or fourth toe causing it to be permanently bent. Some high-impact sporting activities including running, karate, and court sports. Any sport that places undue pressure on the feet. Injuries, an injury or other type of trauma to the foot may lead to a neuroma.
Symptoms
The most common symptom of Morton's neuroma is localized pain in the interspace between the third and fourth toes. It can be sharp or dull, and is worsened by wearing shoes and by walking. Pain usually is less severe when the foot is not bearing weight.
Diagnosis
If you suspect Morton?s Neuroma, it is essential that you confirm your suspicions by consulting with a podiatric physician. Don?t wait for the symptoms to go away for good (even if they tend to come and go). Also, remember that many conditions have similar symptoms, and only a professional can tell the difference.
Non Surgical Treatment
Wear shoes with plenty of room for the toes to move, low heels, and laces or buckles that allow for width adjustment. Wear shoes with thick, shock-absorbent soles, as well as proper insoles that are designed to keep excessive pressure off of the foot. High-heeled shoes over two inches tall should be avoided whenever possible because they place undue strain on the forefoot. Resting the foot and massaging the affected area can temporarily alleviate neuroma pain. Use an ice pack to help to dull the pain and improve comfort. Use over-the-counter shoe pads. These pads can relieve pressure around the affected area.

Surgical Treatment
If conservative treatments haven't helped, your doctor might suggest injections. Some people are helped by the injection of steroids into the painful area. In some cases, surgeons can relieve the pressure on the nerve by cutting nearby structures, such as the ligament that binds together some of the bones in the front of the foot. Surgical removal of the growth may be necessary if other treatments fail to provide pain relief. Although surgery is usually successful, the procedure can result in permanent numbness in the affected toes.
Prevention
Although the exact causes of neuromas are not completely known, the following preventive steps may help. Make sure your exercise shoes have enough room in the front part of the shoe and that your toes are not excessively compressed. Wear shoes with adequate padding in the ball of the foot. Avoid prolonged time in shoes with a narrow toe box or excessive heel height (greater than two inches).
Shoe Lifts The Chiropodists Treatment For Leg Length Imbalances
There are actually not one but two unique variations of leg length discrepancies, congenital and acquired. Congenital implies you are born with it. One leg is structurally shorter compared to the other. As a result of developmental phases of aging, the human brain picks up on the step pattern and identifies some variance. Our bodies usually adapts by tilting one shoulder to the "short" side. A difference of less than a quarter inch isn't very abnormal, require Shoe Lifts to compensate and generally won't have a profound effect over a lifetime.

Leg length inequality goes mainly undiagnosed on a daily basis, however this condition is simply corrected, and can reduce many incidents of back pain.
Treatment for leg length inequality typically involves Shoe Lifts. These are generally very inexpensive, often costing below twenty dollars, in comparison to a custom orthotic of $200 and up. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Upper back pain is the most widespread health problem affecting people today. Around 80 million people are afflicted by back pain at some point in their life. It's a problem which costs businesses millions of dollars annually as a result of time lost and production. Fresh and better treatment solutions are continually sought after in the hope of decreasing the economic influence this condition causes.

Men and women from all corners of the earth experience foot ache due to leg length discrepancy. In these cases Shoe Lifts can be of very helpful. The lifts are capable of relieving any pain and discomfort in the feet. Shoe Lifts are recommended by many professional orthopaedic practitioners".
So that you can support the body in a balanced manner, your feet have got a crucial task to play. Inspite of that, it's often the most overlooked region in the human body. Many people have flat-feet meaning there is unequal force exerted on the feet. This will cause other areas of the body such as knees, ankles and backs to be impacted too. Shoe Lifts make sure that the right posture and balance are restored.

Leg length inequality goes mainly undiagnosed on a daily basis, however this condition is simply corrected, and can reduce many incidents of back pain.
Treatment for leg length inequality typically involves Shoe Lifts. These are generally very inexpensive, often costing below twenty dollars, in comparison to a custom orthotic of $200 and up. Differences over a quarter inch can take their toll on the spine and should probably be compensated for with a heel lift. In some cases, the shortage can be so extreme that it requires a full lift to both the heel and sole of the shoe.
Upper back pain is the most widespread health problem affecting people today. Around 80 million people are afflicted by back pain at some point in their life. It's a problem which costs businesses millions of dollars annually as a result of time lost and production. Fresh and better treatment solutions are continually sought after in the hope of decreasing the economic influence this condition causes.

Men and women from all corners of the earth experience foot ache due to leg length discrepancy. In these cases Shoe Lifts can be of very helpful. The lifts are capable of relieving any pain and discomfort in the feet. Shoe Lifts are recommended by many professional orthopaedic practitioners".
So that you can support the body in a balanced manner, your feet have got a crucial task to play. Inspite of that, it's often the most overlooked region in the human body. Many people have flat-feet meaning there is unequal force exerted on the feet. This will cause other areas of the body such as knees, ankles and backs to be impacted too. Shoe Lifts make sure that the right posture and balance are restored.
What Is A Inferior Calcaneal Spur

Overview
The plantar fascia is connective tissue on the sole of your foot. When the arch of the foot is not properly supported, the plantar fascia can stretch and pull away from the heel area. When the plantar fascia pulls away from the heel, calcium deposits form in its absence. These calcium deposits are called heel spurs and can be very painful.
Causes
Heel Spurs develop when the plantar fascia is excessively and repetitively pulled away from the heel bone. In many cases, a heel spur can develop along with plantar fasciitis, but can also occur by itself. Heel spurs often develop in middle-aged patients, but can also occur in younger people as well. Athletes are especially prone to heel spur due to the regular stress on their heels.

Symptoms
The vast majority of people who have heel spurs feel the asscociated pain during their first steps in the morning. The pain is quite intense and felt either the bottom or front of the heel bone. Typically, the sharp pain diminishes after being up for a while but continues as a dull ache. The pain characteristically returns when first standing up after sitting for long periods.
Diagnosis
Because the diagnosis of heel spurs can be confused with tarsal tunnel syndrome (as described earlier), most surgeons advocate performing a tarsal tunnel release (or at least a partial tarsal tunnel release) along with the plantar fascia release. This surgery is about 80percent successful in relieving pain in the small group of patients who do not improve with conservative treatments.
Non Surgical Treatment
Get some rest. You need to stay off of your aching foot as much as possible for at least a week. Think about possible causes of the problem while you're resting and figure out how you can make some changes. Some actions that can contribute to heel spurs include running too often or running on hard surfaces such as concrete, tight calf muscles, shoes with poor shock absorption. Ease back into your activities. In many cases, you'll be in too much pain to go ahead with a strenuous exercise routine that puts pressure or impact on your heel. Listen to your body and switch to different activities such as swimming or riding a bike until your heel spurs improve.
Surgical Treatment
Approximately 2% of people with painful heel spurs need surgery, meaning that 98 out of 100 people do well with the non-surgical treatments previously described. However, these treatments can sometimes be rather long and drawn out, and may become considerably expensive. Surgery should be considered when conservative treatment is unable to control and prevent the pain. If the pain goes away for a while, and continues to come back off and on, despite conservative treatments, surgery should be considered. If the pain really never goes away, but reaches a plateau, beyond which it does not improve despite conservative treatments, surgery should be considered. If the pain requires three or more injections of "cortisone" into the heel within a twelve month period, surgery should be considered.
Inferior Calcaneal Spur Symtoms

Overview
Heel spurs, or abnormal growths of the heel bone, can cause sharp pains in the heel, especially first thing in the morning and after long periods of rest. In many cases, a heel spur develops as a result of plantar fasciitis, which is the inflammation of the ligament that stretches along the bottom of the foot, from the base of the toes to the heel. In individuals who suffer from plantar fasciitis, the ligament pulls away from the heel as the foot bears weight. In an effort to stabilize the ligament, the body may produce calcium deposits, which can then develop into heel spurs.
Causes
Fctors that increase the risk of developing heel spurs include a high body mass index (BMI), regular vigorous activity, and intensive training routines or sports. Factors such as these are believed to increase the incidence of repetitive stress injuries that are associated with the formation of heel spurs. When a heel spur forms, extremely sharp pain along with the feeling that a part of the heel is trying to burst through the skin usually occurs. If left untreated, an individual may eventually begin to struggle to perform simple activities such as walking.

Symptoms
The pain caused by a calcaneal spur is not the result of the pressure of weight on the point of the spur, but results from inflammation around the tendons where they attach to the heel bone. You might expect the pain to increase as you walk on the spur, but actually it decreases. The pain is most severe when you start to walk after a rest. The nerves and capillaries adapt themselves to the situation as you walk. When you rest, the nerves and capillaries rest, also. Then, as you begin to move about again, extreme demands are made on the blood vessels and nerves, which will cause pain until they again adjust to the spur. If excessive strain has been placed on the foot the day before, the pain may also be greater. A sudden strain, as might be produced by leaping or jumping, can also increase the pain. The pain might be localized at first, but continued walking and standing will soon cause the entire heel to become tender and painful.
Diagnosis
Diagnosis is made using a few different technologies. X-rays are often used first to ensure there is no fracture or tumor in the region. Then ultrasound is used to check the fascia itself to make sure there is no tear and check the level of scar tissue and damage. Neurosensory testing, a non-painful nerve test, can be used to make sure there is not a local nerve problem if the pain is thought to be nerve related. It is important to remember that one can have a very large heel spur and no plantar fasciitis issues or pain at all, or one can have a great deal of pain and virtually no spur at all.
Non Surgical Treatment
Since heel spurs are not an indication of pain themselves unless fractured, treatment is usually aimed at the cause of the pain which in many cases is plantar fasciosis. Treatment of plantar fasciiosis includes; rest until the pain subsides, special stretching exercises and if required orthotics may be prescribed.
Surgical Treatment
Approximately 2% of people with painful heel spurs need surgery, meaning that 98 out of 100 people do well with the non-surgical treatments previously described. However, these treatments can sometimes be rather long and drawn out, and may become considerably expensive. Surgery should be considered when conservative treatment is unable to control and prevent the pain. If the pain goes away for a while, and continues to come back off and on, despite conservative treatments, surgery should be considered. If the pain really never goes away, but reaches a plateau, beyond which it does not improve despite conservative treatments, surgery should be considered. If the pain requires three or more injections of "cortisone" into the heel within a twelve month period, surgery should be considered.